November is National Family Caregiver Awareness Month. David Besst, Co-chair of the Arizona Caregiver Coalition and Dr. David Coon, Associate Vice Provost for Research Collaborations at Health Outcomes @ ASU talk about the valuable service family caregivers provide and the services available to help them.
Ted Simons: It's national family caregiver awareness month. And, as we're about to find out, caregivers are the unsung heroes of our nation's healthcare system. Bonnie Danowski has spent years representing caregivers at the state legislature on behalf of the valley interfaith project. This year, she was named caregiver advocate of the year by the Arizona caregiver coalition. In the following story, producer David Majure and photographer Scott Olson introduce us to Bonnie and her husband, Jim.
Bonnie Danowski: Dinner out tonight, right?
Jim Danowski: Yep.
Bonnie Danowski: Know where you want to go?
Bonnie Danowski: I probably became a caregiver when Jim was diagnosed, which was 41 years ago with multiple sclerosis.
David Majure: They married in 1964. Seven years later, Jim became seriously ill and Bonnie has been caring for him ever since.
Bonnie Danowski: ‘I've got the meetings in the morning'… but I did not self-identify and most caregivers don't, until 12 years ago when he had a serious exacerbation.
Bonnie Danowski: We don't call ourselves caregivers and what happens when that happens, when you do not self-identify, is that all of these crazy feelings go through our heads. God I'm tired. I shouldn't be tired. That person is the sick one. I -- I'm a little resentful today. I shouldn't be, they're the ones sick. I -- I'm -- I'm a little bit angry or I'm feeling grief. When caregivers name themselves and name themselves as caregivers, they then can deal with all of those feelings that come up. Because they're normal, normal feelings.
Bonnie Danowski: The hardest part was to try and live as a normal family because when Jim became disabled, he became disabled and wasn't able to work.
David Majure: The Danowskis had to find a new normal. That wasn't easy. They faced tremendous financial hardships and their social life disappeared.
Bonnie Danowski: I guess that's it. The social and the financial burden. The -- the loss of -- the loss of your friend. The loss of the intimacy of friendship and relationship. That's really hard. And the grieving, people don't really identify it as grieving, usually. But the grieving goes on and on and on. We think of grief as when someone dies or something, but when a person who has an illness like my husband, or a stroke, each time they lose one of their abilities, you grieve that. Because there's another part of the person lost. But the essence of the person is always there and that is what keeps the relationships together.
David Majure: They say love is blind and quite often, family caregivers are unable to see how their selfless act of caring is impairing their own mental and physical health.
Bonnie Danowski: It takes a toll. There were times when I was taking more medication than Jim was. So -- because I wasn't taking care of myself. And that's the reason I advocate for family caregivers, because I know they don't. We don't do it, and we need to. Because if we fall apart, you know, then who is going to take care of that person, besides that fact, we are, as individuals, important in -- and we need to honor ourselves and take care of ourselves. Period. So --
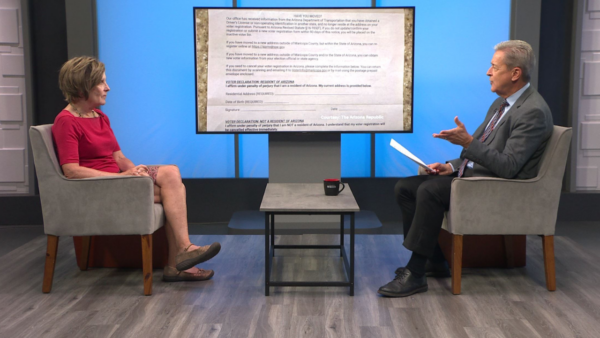
Ted Simons: Joining me to talk about services and support available to family caregivers is -- David Besst, a caregiver support specialist for the Arizona DES division of aging and adult services. He's also chairman of the Arizona caregiver coalition. And professor Dr. David Coon, associate vice provost of health outcomes at ASU. His research is focused on helping caregivers manage stress. Good to have you here.
Ted Simons: Is the Bonnie story familiar?
David Besst: Very familiar. And it's all too typical what she said about self-identification, because it's typically one of the biggest challenges we face is having caregivers actually recognize the situation they're in.
Ted Simons: When is it time for a family caregiver to realize, maybe I need some help? Maybe some respite care is what's going on? I mean, how do you know?
David Besst: It's tough actually and there's a couple of things we're doing right now in Arizona that are really important in that regard, in that we -- with Dr. Coon's help and ASU's help as part of our -- and ASU's help, when we encounter clients that call into DES or one of the agencies on aging, for example, and that tool is used for anyone that gets respite and on our website, www.AZcaregiver.org, there's a link to an AMA self-assessment tool, which is a good tool that will give a caregiver where they stand in that continuum and where they need help.
Ted Simons: How much of -- how much can you quantify something like this?
David Coon: It's very hard to exactly quantify it. I think we're looking at what are key characteristics, lack of sleep, irritability. People not being able to respond in the way they did before, work performance impact. Financial strain. A lot of the things that Bonnie talked about, these are -- caregivers are the hidden patient. They're truly impacted, they're stepping up to the plate because we love and care about this individual, but the reality is it impacts the context in which they live. As far as your research, what are you seeing? How often do these scenarios play out? Are other family members doing their part, not just in helping with the relative, but telling the caregiver, you need time for yourself here?
David Coon: I think unfortunately, more times than not, it tends to fall on one person's shoulders. One person steps up or becomes identified because of their own life circumstance. Perhaps living with a parent. An adult child, or it's the spouse. And we know from the research is the reality that spouses are much less likely to identify themselves as a caregiver than the adult child that find themselves running across town to take care of mom, the neighbor called and complained there's smoke, mom left the stove on and it's starting to have -- is starting to have more and more memory problems. The parent -- the spouse, rather -- it's what I do. I've always done this for your dad. So they have a more difficult time.
Ted Simons: Someone is watching, you know what? I need help here. A family member could be watching, saying, I think dad, mom might need help. What help is available?
David Besst: There's a variety of support services. My primary job with DES is overseeing the national family caregivers' support program which comes out of the aging community but with programs like lifespan respite, lifespan denotes it's not caregivers of aging people. But also people that are caring for children with special needs or caring for their spouse, like Bonnie, that would not qualify for aging program funding, so what we're try doing is develop a collaborative process so we can bring together the resources available to caregivers and make it easily accessible and that's one of the things that the coalition is trying to do.
Ted Simons: What are the resources that you would like to see emphasized most?
David Coon: There's clearly -- emphasized. But more and more what we see and know from our research and the reasons we develop programs we do, often they need skills in managing stress and the behavior problems that might come along with dementia. We've developed partnerships with David's group and the Alzheimer's association and the area agency on aging to teach people how to communicate in their families and manage the situations more effectively.
Ted Simons: We were talking unpaid caregivers, talking $9 billion in services every year in Arizona. Alone.
David Besst: It's a pretty amazing thing. It breaks down to about 80% of all of the in-home care provided that keeps people living at home independently. 80% of the care is provided by a loved one for no compensation. It's easy to see if you took away that -- that prominent form of support, that's why we need the support -- to support caregivers because they provide most of the actual support for those trying to live independently outside of facilities.
Ted Simons: Last question -- Go ahead.
David Coon: Our whole long-term care system would collapse if we had to pay for this.
Ted Simons: What do you folks to take from this, to understand?
David Coon: I think it's critical they begin to recognize the family members that are providing care and how if they're the primary person, they reach out. If they're a person not providing the care, what can they do? You can mow the lawn for mom, so she doesn't have to worry if she's taking care of dad.
Ted Simons: Good conversation. Thank you for joining us.
David Besst: Thank you.
David Coon: Thank you.
David Besst:Co-chair,Arizona Caregiver Coalition; Dr. David Coon: Associate Vice Provost for Research Collaborations at Health Outcomes, Arizona State University;