American Rescue Plan Act adds new rules to COBRA
May 5, 2021
COBRA or the Consolidated Omnibus Budget Reconciliation Act gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods under certain circumstances such as voluntary or involuntary job loss, reduction in the hours worked, a transition between jobs, death, divorce, and other life events.
New COBRA rules just went into effect on April 1st, providing a federal subsidy of COBRA premiums through September 30th. As part of the American Rescue Plan Act of 2021, involuntarily separated employees will not have to pay the exorbitant, and often prohibitive, COBRA premiums to keep their health insurance. Employers will have to advance these premiums and then will be reimbursed in the form of quarterly tax credits.
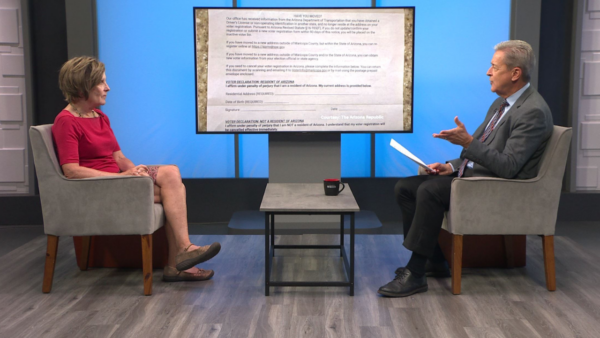
We talked with Kristi Lundstrom Hill from Fennemore-Craig about these changes, and everything people will need to know. Lundstrom-Hill explains further what COBRA is and what it can do for people. She said the maximum period for COBRA is 18 months. It requires employers to pay the cost of the COBRA coverage for a “certain group of employees.” The employers are then reimbursed by the Federal government.
She explains that the changes to COBRA are intended to help people that lost their jobs maintain health coverage at no cost to them. Although, she said the IRS has not yet released guidance on exactly how that will work.
Lundstrom Hill said that anyone that loses their job or has reduced their hours enough to lose coverage would be covered under COBRA. She goes into the details on COBRA and who is now eligible for COBRA. She said people that ended COBRA early can even jump back in. COBRA has changed, but the new rules do not “override” any of the existing COBRA rules. She said it is an “additional burden on employers but doesn’t change the rules that are already there.”