state lawmakers have formed a joint select committee to investigate operations and conditions at the nursing home for veterans in Phoenix. Committee members Rep. John Nelson and Rep.Ben Miranda discuss the legislative hearings.
Cary Pfeffer:
Health care for our country's veterans is in the national spotlight while here at home the Arizona Veterans Home has state lawmakers busy. We talk with legislative panel members.
Cary Pfeffer:
If you're sneezing and suffering from allergies, now more than ever you are not alone. We talk with allergy doctors about this whopper of an allergy season and what you can do for your own allergies. Those stories next on "Horizon."
Announcer:
"Horizon" is made possible by contributions from the friends of eight. Members of your Arizona PBS station. Thank you.
Cary Pfeffer:
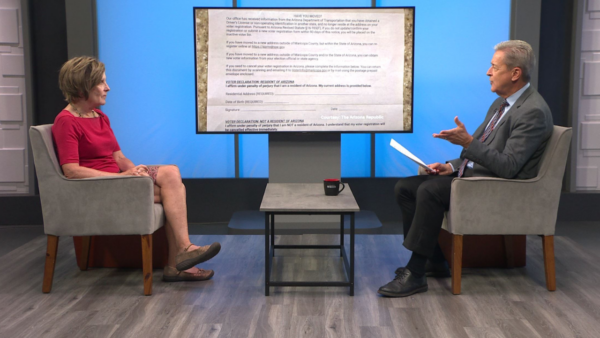
Good evening. I'm Cary Pfeffer. Welcome to "Horizon." Legislative hearings continue on the Arizona Veterans Homes. State lawmakers formed a joint select committee to investigate operations and conditions at the nursing home for veterans here in Phoenix. The committee began hearings at the state Senate last week, looking into patient neglect at the Veterans Home. Those hearings have now been moved to the House of Representatives. Committee Co-Chair Representative John Nelson joins us. Also here is committee member Representative Ben Miranda. Thank you both for being here. We appreciate that. Representative Nelson, we'll begin with you. First of all we should lay out a little bit of groundwork because we can't assume everyone is up to date on all of this. In mid- to late March we learned about difficult conditions, some found troubling conditions at the Arizona Veterans Home. That's when this process got started, correct?
John Nelson:
Well, the process got started earlier than that. When you got into the actual inspection, it didn't hit the public until later. It was in early February -- mid February when the D.H.S, Department of Health Services went in and did an inspection and found that there were some -- five or six problems in there. That one was a very extreme position or situation because it involved smoking in the Alzheimer's unit that had people that were using oxygen. The alert was sent out, and they started dealing with the problem at that time.
Cary Pfeffer:
Then it was a matter of the lawmakers getting involved, and Representative Miranda, why don't you talk a little bit about what some of the original goals were in putting this joint legislative committee together?
Ben Miranda:
I think the charge was to look at the facility, determine exactly what the violations that were revealed indicated, as you know the governor has also had a corrective action, plan in place, determining whether anything additional needs to be done to correct the problems. We have a charge. The charge is to look at the problem and try to see what can be done and to see what was -- what occurred that was wrong. If something else could have been done during that time and to point that out.
Cary Pfeffer:
This has become a national issue because of work done by "The Washington Post" and discoveries that were made back on the east coast about substandard veteran care, so it becomes even more the focus of attention. Representative Nelson, there was part of this playing in the background questions about who knew what and when they knew it, what part should that play in what's happening with this committee?
John Nelson:
You have two phases. You're talking about what I consider the administrative phase. It was staff's duty to notify and in this case Director Gerard had notified the governor's office around the 10th of February. There seems to be a time lapse in the communications between staff and the governor, and the question is how much of a problem did that create because there were obvious -- we had some problems at the facility. There were claims of nepotism and some other things going on there. If they had taken that to the governor and gotten directions earlier maybe some of those issues would have been solved, it wouldn't have become as explosive as it has now.
Cary Pfeffer:
So the question is, were delays possibly adding to the problems.
John Nelson:
Yes. The other side of that is from what I have read and seen, we have got good staff at the facility, and I don't want the public to think differently. They have worked hard. They did their assessment. They came up with an improvement plan and they are working on that. I think that has been accepted. It was accepted a week ago when we first started meeting by D.H.S., so there's a partnership between D.H.S. and the facility. We get no new patients until we resolve this, which has an impact on the monies coming into the home and the services we can deliver.
Cary Pfeffer:
Representative Miranda, is this a situation where some of these outside issues, like I said, who knew what and when they knew it, does that need to be part of this discussion in your estimation?
Ben Miranda:
I think that we focus in, which we have, unfortunately in my opinion, on emails that have floated back and forth, I think to a certain degree I think it's helpful. I think it is necessary for us to delve into those issues, but for the most part I think that if we understand the timeline that's involved here, for instance the survey was done on February 9. The most serious problems were corrected by February 12, which seems to me a reasonable timeline to have done it in. The question becomes after February 12 not what this committee is now focusing in. I'm not in complete agreement with focusing in on all the emails floating back and forth. I don't think that does us any good to correct the problem. I think frankly it leads to a source of tension between the two parties when in fact it shouldn't be. Shouldn't be partisan. It should be a nonpartisan effort to try to look at this effort and correct the problems.
Cary Pfeffer:
Representative Nelson, we're seeing a situation where this hearing has been moved from the Senate to the House. Is that part of that effort to move on?
John Nelson:
Well, technically, we were supposed to be in the Senate and then the House, move back and forth. The decision was made to stay in the Senate because of the events that occurred, and now it's in the House, and the next two meetings will be there. It looks like I'm going to have a couple of members missing, so we may wind up moving the meeting into next week. Try to finish it up then. But it still comes down to at least at the hospital that I serve on the board on we have an administrator and then we have presidents above that or vice presidents that look down on what happens at the facility. If you get nailed too hard, they are down on your back trying to figure out what's happening. I don't think this is and should be assumed to be anything different than that. The private sector does it. If the public sector does it it's a repetitious event.
Cary Pfeffer:
In other words you're not wanting to complicate the matter more by taking specific actions that could sort of slow some of the progress?
John Nelson:
I'm not saying slow it, but I think from my perspective divided into two positions. You have your administrative end, which is responsible for the functions that go on. Ours was separate. It was down literally at the capitol. The day-to-day operations were covered by an administrator who I don't know what the lines of communications were, and then we had a V.A. inspection a month before that, there were some carry-forward items in there that did not get resolved in that 30-day period. So why didn't that happen? We had better lines of communications between the facility and the administration; maybe we wouldn't have had these kinds of problems. Or as severe. I don't want to try to dump everything.
Ben Miranda:
I think it's important to focus in on what we need to do for veterans. What we need is have an improved facility and make sure that lines of communication as John has indicated are improved if they need to be, and improved from the perspective of communicating those reports, those surveys that are done and making sure whether it be the governor or the survey that's done, communicated to the staff, but I think it's important to focus on what we need to do and to improve the life of those veterans. After all, they deserve better than they have received in the past.
Cary Pfeffer:
Let's move on to that part of it. It seems like there may be some specific sort of concrete recommendations, Representative Miranda if you could say what direction you would like to see the committee go and then we'll ask Representative Nelson.
Ben Miranda:
I don't want to speculate too much on where we're going, but I will say that it appears to me that we're understaffed; it appears to me that the staff is not adequately paid. I think if we're going to get some reports I think hopefully in the next few hearings that indicate whether or not how they compare private and public sector. I think those are all going to be fleshed out. I think the end result is going to be that you have under staff problems. The training of staff is directly related to what you pay them. I think we're going to need to take some actions to correct that and funnel more resources into those facilities.
Cary Pfeffer:
If you could assess, Representative Nelson, would you agree or add or subtract from that list?
John Nelson:
You could pretty much agree. It's a matter of service, what's available in the community, the difference between the private and public sector pay. There were comments that we train them and they go somewhere else. But the turnover rate at the facility is pretty low. I think it was down in the 10, 15% range, which that is pretty low for what I have seen at the hospital in the past. So if that is the case, we have got good staff. If we have some that aren't doing what they need to do, we obviously need to either train them or move them on. I tend to agree with Ben on the operations of the facility and coming up with something that is consistent. It appears that they have resolved the call button situation.
Cary Pfeffer:
Where somebody had apparently not been able to get help and was found -- and was neglected basically.
John Nelson:
Yes. Through the day you're getting a 15-minute reminder to check your call buttons. They are dealing with the other issues I think one has been appealed and probably upheld, but the others they created their action plan, they will go through and work that out, take it back to D.H.S., if it's in agreement that will take this issue and move it on. But they still need the recommendations of what we do on the staffing side, what comes down with funding.
Cary Pfeffer:
Right. Some of it dollars and cents.
Ben Miranda:
I think I'm happy to see the hearing go back to the House. I think John is an excellent chairman. I have seen him chair committees before. I think we'll get better results from having it in the House.
Cary Pfeffer:
Just to follow up briefly on the pay scale issue because I think people might be helped and enlightened by this process. First of all it's not easy to find qualified folks. Secondly, we're talking not about R.N.'S, registered nurses taking care of these folks, but they are instead folks making about $8 or $10 an hour. Can you explain the level of training or where that stands?
John Nelson:
That's a little bit beyond me. Just to be straight, but with one of the -- the $8 to $10 is dollars is purely dollars across the board. That doesn't count benefits which range up to about 30%. We're not the poorest or cheapest around. I think. But I agree with what Ben is saying. We have to take care of our veterans. I have two uncles that died in an old soldier's home about 30 years ago. If you think about that, that these people are laying in there, some immobile, some not able to get themselves from their bed to their bathroom, bed to the toilet, pushing the button when you gotta go and you can't get help -- we have to take care of those situations.
Ben Miranda:
I think again we'll see whether these are systemic or episodic problems. That gets to the heart of the issue. I strongly believe that they are on a good road right now. I think the staff -- I agree with John, the staff is excellent at that facility. If it needs additional training I think it will be looked at. I think it's going to happen over the next few months, need be throughout the year. I am a veteran. John is a veteran. We're both veterans. We both have a vested interest in trying to take care of those folks.
Cary Pfeffer:
If it comes down to dollars, is there the will to get that addressed?
Ben Miranda:
Certainly there's a lot of pressure in the legislative process to provide those bucks now.
Cary Pfeffer:
Yes. It seems that that would be the case just with the attention that's been shown. Yes.
Cary Pfeffer:
Representative Nelson, Representative Miranda, appreciate you being here and helping us understand this issue a little bit more and giving us an update on where it stands. We appreciate it. Thank you.
Ben Miranda, John Nelson:
Thanks for having us.
Cary Pfeffer:
Are you suffering from watery, itchy eyes and runny nose? Have you been coughing, perhaps congested? Well if so, you may be among the thousands of allergy sufferers in the valley feeling the pain this season. The strong breezes and cooler temperatures don't help matters very much. Aside from the over-the-counter drugs that are available, there is some relief for serious allergy sufferers out there being properly diagnosed is a start. We'll talk more about that in just a moment. First Merry Lucero tells us why allergy symptoms may be worse this season.
Merry Lucero:
Spring has sprung. Flowers are blooming. From mesquite to olive, blossoms are everywhere. For allergy sufferers that means one thing. Pollen. For chronic allergy patients like Richard Vezzosi, it means more time at the doctor's office.
Richard Vezzosi:
This is the worst this year for me. Why, I don't know. It's worse this year. As far as my breathing.
Merry Lucero:
Dr. Bart Leyko thinks this year is somewhat worse than last year in the valley. A series of sharp climate changes is fueling allergens.
Bart Leyko:
We have patients with more symptoms this year. I think the weather also was such that the plants held off with pollen release because of the cold weather, and when the heat came in, along with the rain, rain which stimulates the plants to release pollen, we had a large amount of pollen released around the same time.
Merry Lucero:
Multiple plants, grasses, weeds and trees are pollinating. Many people are coughing, sneezing and feel more tired and achy than they ever have.
Bart Leyko:
Many patients that have allergies may have some reactive disease we call it and maybe before it wasn't so apparent or was slowly developing, getting worse, and this allergy season it's certainly finally -- it can be diagnosed, because the symptoms became so severe.
Merry Lucero:
Allergies cause inflammation of the airways as in Vezzosi's case; this can lead to asthma, bronchitis and sinusitis.
Richard Vezzosi:
I get the wheezing, can't breathe, I get a sinus infection. Lungs are real bad. That is are the kinds of things, I have trouble breathing at night really bad.
Merry Lucero:
People with allergies tend to get more viral and bacterial infections. Why?
Bart Leyko:
Probably because the immune system is busy fighting the allergies and you get the baseline inflammation and you get swelling of the airways, mucous production that makes it harder to resist the viral infection. In fact that may provide a ground for a bacterial infection. It tends to provide more food in terms of the mucous and swollen airways. Makes them more exposed to viral infection.
Merry Lucero:
Pollutants or other irritants can also cause those ailments. As for allergies, medications can counteract the inflammatory reaction.
Richard Vezzosi:
I'm taking allergy shots and all the inhalers and stuff like that. Flonase, Advair a bunch of them. They do help to a point, but this time I can't -- nothing was helping me. So he will give me something special, maybe a prescription and that will usually clear me up. I'll be all right for a while, and it will come back. Just with the change of season. There isn't much you can do about it.
Merry Lucero:
Desensitization is another prescription.
Bart Leyko:
We desensitize a person to the allergen through a repeated injection of increasing quantity of the allergen at the time. It's a long process, but probably the closest thing to a cure that we have for allergies.
Merry Lucero:
Indoor allergy triggers can be reduced, but outdoors, controlling pollen is difficult because it travels for miles, making allergy patients sick.
Richard Vezzosi:
I can't breathe at night hardly at all. I use all the products they told me to use. I just get so congested. I just can't -- hopefully he will help me today.
Merry Lucero:
In the meantime Vezzosi and other allergy sufferers hope someday to be able to stop and smell the flowers.
Cary Pfeffer:
Recently I spoke in detail with Dr. Mark Schubert of the Allergy Asthma Clinic about causes, treatment and continuing care of allergies.
Cary Pfeffer:
Thanks for being here. Let's start with the undeniable fact that this has been a very difficult year for people who suffer with allergies. I'm sure Kleenex sales are through the roof.
Cary Pfeffer:
We're in a situation where this year as compared to maybe some recently really is a difficult one.
Mark Schubert:
I think every year seems to be getting somewhat worse. The existing trees are getting bigger. So more pollen per tree, although we have done a few things to try to limit growth of some of the major pollen producers, but nonetheless, I think each spring seems to be getting worse.
Cary Pfeffer:
Sometimes there are factors that happen as far as temperature and that sort of thing that can have some impacts on what it's like year to year?
Mark Schubert:
Sure. I think we do see pollen counts sometimes higher, the next year lower, higher. There seems to be a cycle. The over all pollen counts are rising a bit with the exception of Olive and Mulberry tree.
Cary Pfeffer:
Let's pick up on that. You are part of an effort in the early '90's to try to limit the kinds of specifically Mulberry and Olive trees that were so much the source of a problem for folks like me who suffer from these things.
Mark Schubert:
That's right. Paul Johnson, the mayor at the time, asked some of us to review the literature and take a look at what we had in the way of pollen counts locally to make a decision as to whether or not there should be anything done about limiting any tree or plant. After looking at it carefully we did decide that Olive and Mulberry were the best candidates to really limit. We did write a law that did pass through the city of Phoenix as an ordinance, and then through Maricopa County Association of Governments, MAG, the surrounding cities picked up that ordinance. We have banned all of the Mulberry tree plantings since about '92. The existing trees of course are grandfathered in, but with the growth of the valley, certainly I think this is having an impact by not adding additional new trees.
Cary Pfeffer:
Do you have a sense, now we're more than ten years into that process, do you have a sense that, well, the population has grown, certainly we have planted a lot of other things, we had just continued with those Mulberry and Olive plants out there we would probably be in worse shape than we are now?
Mark Schubert:
I think it would have been a disaster. Both Olive and Mulberry pollens are very serious allergy producers. That's why we banned those two specifically. It takes about 20 pollen grains per cubic meter of air to cause allergy during the allergy season. Olive tree makes about 300 and Mulberry tree makes about 3,000.
Cary Pfeffer:
Wow. Now there's some talk about sort of expanding some of that, trying to search out -- we know what the top two culprits were. Is there some thought of maybe even considering some other plants that are difficult for us?
Mark Schubert:
There isn't right now. That would require a further initiative. But when you look at the pollen count data as I have, that we really had during those years, it was Olive and Mulberry that really stood out. Some folks would like to ban, for example, Bermuda grass. I think Bermuda grass is now an indigenous grass. It grows wild everywhere. It still is a popular grass for lawns. I think it would be very difficult to try to really ban that grass.
Cary Pfeffer:
Let's move on to some of the things that can be done for somebody who is suffering. Certainly there are people who are watching this program who are saying, that's me. I can identify with the sniffles and sneezing and just feeling zapped of energy. Talk about some of the treatments out there as well as the skin test that's now available.
Mark Schubert:
Treatment does follow directly on diagnosis. A lot of folks think they may have allergy. In fact when you ask 100 people to raise your hands how many of you have allergies, about 50 to 80 will depending on the study. But actually we know that about 35 have allergy. The rest of them have other forms of non-allergic nasal sinus disease. But, skin testing will give us the answer if a patient is symptomatic. Will tell us exactly what the problem is, and based on those results we can follow right into treatment.
Cary Pfeffer:
When people think of a skin test, for anybody in my age group, they think of the old fashioned skin test which was pretty elaborate and took a pretty long period of time. The good news is that that test has been updated and it's not nearly as sort of feared as it once was.
Mark Schubert:
Well, thank you for pointing that out. I appreciate that. It's true. Allergy skin test has been streamlined. Now we use a little plastic device where we place little water droplets on the forearms, make a tiny prick right on the surface level of the skin, it's just a touch actually you can feel it, but it's not painful. It takes just a few moments to put these little drops on. Each drop has a different pollen in there and within 20 minutes you'll see an itchy little red welt come up if you're allergic to something specific. We make a list and then we just wipe them off.
Cary Pfeffer:
That's nothing compared to sort of the old fashioned way. Let's lastly talk about some of those specific treatments that people should consider. There really are -- they fall into sort of three categories.
Mark Schubert:
We have three categories of treatment. We've got avoidance, avoidance based upon knowledge of exactly what you're allergic to.
Cary Pfeffer:
Staying away from whatever that is.
Mark Schubert:
Right. Allergy skin testing will give you that information. Avoidance can't really be a full treatment unless it's something direct like cat allergy only or dog allergy only. Then you've got avoidance strategies you could. But then you have pharmacotherapy medications and then the third category is immunotherapy or allergy shots.
Cary Pfeffer:
When someone comes into the office you lay out those possibilities and it's a matter of having that discussion with the patient.
Mark Schubert:
That's right. Most patients are going to be on some combination of those three categories although some as I say may do fine just with an avoidance strategy, but most will require, by the time they come to an allergist they're severe enough, they require some combination of treatment.
Cary Pfeffer:
Alright. Dr. Schubert thanks very much. Appreciate you coming in.
Mark Schubert:
My pleasure. Thank you.
Larry Lemmons:
If you operate a business licensed by the town of Payson, make sure your workers are in the country legally. A new town ordinance seeks to revoke the licenses of businesses who repeatedly hire illegal immigrants. See how town residents are responding and find out what the state is doing about employer sanctions Wednesday at 7:00 on "Horizon."
Cary Pfeffer:
Thanks very much for joining us. Have a good night.
Announcer:
If you have comments about "Horizon," please contact us at the addresses listed on your screen. Your name and comments may be used on a future edition of "Horizon."
Announcer:
"Horizon" is made possible by contributions from the friends of EIGHT, members of your Arizona PBS station. Thank you.
John Nelson:State Representative;Ben Miranda:State Representative;