HealthTell Inc., a biotech spinout from Arizona State University, has raised $4 million in new funding to help commercialize a new test for lung, breast, prostate and colorectal cancer. The HealthTell diagnostics technology was developed at the ASU Biodesign Institute in part by Dr. Stephen A. Johnston, who will talk about the new test and the funding.
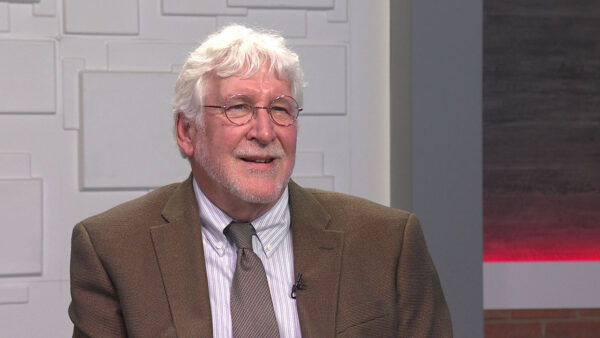
Ted Simons: HealthTell is a local startup medical company that worked with ASU's Biodesign Institute to develop a test that can detect cancer and more than 30 other illnesses by measuring the body's response to a pathogen instead of attempting to detect the pathogen itself. Dr. Stephen A. Johnston developed the new test. And he joins us right now. Thank you so much for being here. This is a new test for cancer. Give us more here.
Dr. Stephen A. Johnston: Well, our goal has been to have a really simple, inexpensive test that would work for any disease. And we have been working on it for many years to do that. The process is quite simple. You take a drop of blood, literally a drop, and you dilute it 10,000-fold and you put it on a little chip that we manufacture. And what happens is, your antibodies that are in your blood bind to that chip. We wash it off and we look at signature, basically the fingerprint of your antibodies on that signature. And it changes day to day but it also changes coherently if you have a particular disease. So the signature, when you have a cancer, will change versus Alzheimer's.
Ted Simons: This is lung cancer, breast cancer, prostate cancer, colorectal, all the biggies?
Dr. Stephen A. Johnston: We have looked at all of those.
Ted Simons: How do you test the test? How do you know it works?
Dr. Stephen A. Johnston: So fortunately there are many registries where they have collected blood on people who had a particular kind of cancer and people that don't have that cancer. Because this assay is so simple we can go back to those blood collections and say, OK, can we tell the difference in the blood between somebody who has breast cancer and somebody who doesn't have breast cancer, somebody who has lung cancer versus somebody who has breast cancer, and it's a very simple test. We can pretty quickly figure that out.
Ted Simons: Black and white or is there some gray areas?
Dr. Stephen A. Johnston: There are gray areas because cancers have different stages. And some of them are earlier than others. And so for instance when we looked at very early pancreatic cancer, the signature of that looks very different than late-stage pancreatic cancer. Cancer is changing even over time.
Ted Simons: But do both signatures, are they both different from no pancreatic cancer?
Dr. Stephen A. Johnston: Yes.
Ted Simons: So you know something is going on, just not maybe sure what?
Dr. Stephen A. Johnston: Right. And we can figure that out, it just takes longer. We have to look at more samples and look at it more carefully.
Ted Simons: This business of an immuno signature, what are we talking about here?
Dr. Stephen A. Johnston: It's basically what I described. You have about 100 billion antibodies in you at any particular time. And they are changing all the time relative to your health status. And so when you get a cancer, or Alzheimer's, or an infection, one of the first things that happens is that the cells that make those antibodies change their production rates and what they are making. And the chip that we designed is so sensitive it can actually pick that up, those small changes that are taking place, even at early stages of cancer and infection.
Ted Simons: Is it similar to when people get tested for viruses? They find antibodies. If you had chickenpox or mumps when you were a kid, you will have those antibodies with you the rest of your life.
Dr. Stephen A. Johnston: It's the same principles, the same antibodies being tested but in the old ways, we just collected the sum of those and we said, OK, you have antibodies to chicken pox. Now we can spread all of those antibodies out and look at them in their fine detail and basically tell, you have a good protection against chickenpox or you don't have good protection against chickenpox.
Ted Simons: With that in mind can you look at this test and say, you don't have pancreatic cancer or whatever the case may be, but the immuno signature suggests you might or the tendency is there. Does it work that way?
Dr. Stephen A. Johnston: No, it doesn't. That's more the 23andMe type of assay where you look at the DNA and you say, oh, you have a genetic mutation that makes you more likely to get this cancer. What this would be more than the next stage where you say, maybe I have a propensity for lung cancer, but that doesn't say I will get it or even when I will get it. But you would use this test if it all works the way we plan it, you would use this test to say, OK, now I see that there is the first indication of lung cancer.
Ted Simons: And compare what this test would do with current detection methods.
Dr. Stephen A. Johnston: We have very, very few what are called biomarkers for early cancer detection. So really what we are trying to push this for is that we can take the time point that you would detect a cancer earlier and earlier. We know, from a lot of, for a lot of experiments, that cancer can start 10 or 20 years before it's actually diagnosed. But we don't have those markers yet that we can pick that out. We think these immuno signatures because they are so sensitive may allow us to do that.
Ted Simons: It's interesting you bring that up because there was some debate I think with men's prostate cancer especially regarding a test whether or not you need to know you have it when it could be 20,30,40 years in development, and you could be long gone by the time this becomes a problem. How does that play into all this?
Dr. Stephen A. Johnston: That's a really important question. It plays very prominently in the question. These are called -- it's estimated that for prostate cancer, breast cancer, lung cancer, there's maybe 25 percent of the growth that you won't even call them cancers, growths that are detected by current diagnostic techniques are actually something we shouldn't worry about. They will either self-resolve or they will stay indolent for, stalled for so long that they are not even a concern. So an important aspect for any detection system that's going to detect cancer early is to be able to tell the good guys from the bad guys. And that's an important challenge for us.
Ted Simons: A challenge but can that challenge be met?
Dr. Stephen A. Johnston: We think it can and our preliminary evidence says that that's certainly a possibility, to tell what is an aggressive cancer from a benign cancer.
Ted Simons: Technology designed at the ASU Biodesign Institute. Give us more information on that.
Dr. Stephen A. Johnston: The institute or the technology?
Ted Simons: The whole process. I was hired about seven years ago by George Post to come over here and invent things that nobody would take a chance on. That's what I did. And the Biodesign Institute was the place to go for doing that, to do way-out ideas and they gave you a running chance to see if you could do it or not. And it's turned out quite well. The ideas that George let me try out that everybody thought was crazy, they look pretty promising right now. This was one of them.
Ted Simons: Was this an idea you had?
Dr. Stephen A. Johnston: Yeah.
Ted Simons: Or idea you researched?
Dr. Stephen A. Johnston: No. It's an idea, it was driven by the concept that we had to revolutionize health care. We can't have, we can't be going on -- I have heard the talk just before this, and the health care act is good in the sense, or bad, depending on your opinion, but it basically redistributes who's taking responsibility for the current system. What we really need to do is fundamentally rethink the health care so we stop being a post symptomatic health care system taking care of people after they get sick and start being presymptomatic so we can give people better costs cheaper. That was our mission, can we get, is there a technology we could invent to allow people to have better health care cheaper, and cheaper is important.
Ted Simons: Indeed.
Dr. Stephen A. Johnston: It wasn't then. We got criticized for saying the word "cheaper." But that was the sole goal. We just set out, I am an inventor, and so I just said, that's the goal. Let's see what we can invent and what we came up with was immuno signatures.
Ted Simons: This is licensed through ASU tech transfer arm? Explain please.
Dr. Stephen A. Johnston: All of the technology that's developed by people within ASU goes through an independent entity that watches out for ASU's intellectual property called AZT. They go out and say here's the technology. We will contact the people that might be invest in it or license it or something. They are basically the technology transfer managers for all of ASU.
Ted Simons: Interesting. So we got this new test now. Is the new test in use?
Dr. Stephen A. Johnston: No. So that's what health care or HealthTell was started for.
Ted Simons: OK.
Dr. Stephen A. Johnston: So we need to, there's an important aspect of that. I briefly went over this chip. Right? The key is that if you are going to monitor people's health on a regular basis, every let's say once every six months or something, you have to be able to manufacture millions if not billions of these chips. So we turned to the Intel-type technology to start manufacturing these chips and just set up a facility in Chandler to manufacture these chips on a large scale.
Ted Simons: Real quickly, one year away? Two years away?
Dr. Stephen A. Johnston: The launch estimate is the beginning of 2015.
Ted Simons: All right. Good luck. Encouraging news and we wish you the best.
Dr. Stephen A. Johnston: Thank you very much.
Dr. Stephen A. Johnston:ASU Biodesign Institute