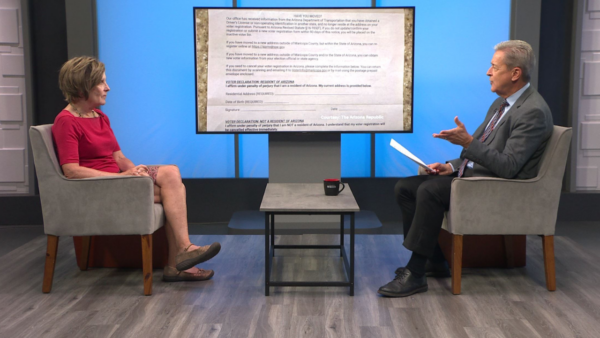
Dr. Laura Nelson, Acting Director of the Division of Behavioral Health for the State Department of Health Services talks about implementing state budget cuts, and how they may impact people with serious mental illnesses.
Ted Simons:
State budget cuts will have a profound impact on many Arizonans with serious mental illnesses. This week, the Arizona Department of Health Services released guidelines for dealing with the cuts. They include plans for a statewide behavioral health crisis system, reduced benefits for the seriously mentally ill who are not Medicaid eligible and housing services for SMI adults who do qualify for Medicaid. Here to talk about that is Dr. Laura Nelson, Acting Director of the Department of Health Services Division of Behavioral Health. Good to see you. Thank you for joining us. Let's get the basics here as far as the budget cuts are concerned. We're talking 50-some-odd percent here?
Laura Nelson:
Yes, over 50 percent reduction in the state general fund dollars that went to support individuals who don't qualify for Medicaid, including adults with serious mental illness.
Ted Simons:
What kind of numbers are we talking about here?
Laura Nelson:
We went from about $127 million total in the general fund to support children and adults that don't qualify for Medicaid down to about 60 million. Since fiscal year 2008. We've gone from about 90 million to serve adults with serious mental illness down to about 40.
Ted Simons:
So let's talk about some of the ways the state is trying to, and providers, are trying to stretch these funds.
Laura Nelson:
We need to figure out how to make these dollars last the entire year, so we're looking at how we can provide the best services and the most economical way. The service package is essentially being changed from a full array of covered services, including transportation, residential services, in-patient facilities, to medications only and access to a physician to prescribe those medications.
Ted Simons:
And I want to get to medication in second here, but as far as case management and transportation and job training and these sorts of things, how much is really being cut back here?
Laura Nelson:
Essentially, all of it, if you are an adult that doesn't qualify for Medicaid. If you were found an adult with serious mental illness, you were entitled to the full array of benefits, it didn't matter if you qualified for Medicaid or not, but now it does. It is shrinking to medication only and doctors. No transportation, no case managers.
Ted Simons:
That's got to hit the rural areas especially hard.
Laura Nelson:
Absolutely. We've spent the last month reaching out to all 14,000 of these adults with serious mental illness around the state to rescreen them for Medicaid eligibility for access and for others we will spend May and June to meet with them individually, one on one, to look at services they've been receiving and how we can safely transition them to this reduced package.
Ted Simons:
You mentioned Medication; I know this is especially important for a lot of folks with serious mental illness. It sounds as if brand names are going to have to be out the door here in favor of generics. True?
Laura Nelson:
It looks like it at this point. We're continuing to investigate other opportunities through some of the pharmaceutical companies. They offer some prescription benefit programs. We're looking at those. There are some individuals who may actually have another source of insurance, like Medicare or VA benefits. In those cases, they may still be eligible for some of the brand name medications. There are also some discount pharmacy cards we may be able to tap into to offset the costs.
Ted Simons:
That has to be a concern because I know for a lot of conditions, those brand names, they don't have generics and some has to be the medication of choice.
Laura Nelson:
Absolutely. There are quite a few newer atypical anti¬psychotic medications that treat things like schizophrenia and bipolar disorder that aren't available in a generic form yet. There are still alternative medications that treat the same symptoms but everyone responds to medications differently so it is nice to be able to have a variety of options.
Ted Simons:
You mentioned in-patient care, crisis treatment. Again, correct me if I'm wrong, up to three days, okay, after three days, what? Out of pocket? What happens here?
Laura Nelson:
We don't have enough funding here, we do not believe, to support a crisis stabilization admission that would be longer than three days. What we are building into this crisis system package would be access to toll-free crisis lines so you could call if you needed crisis assistance, mobile teams that could come out and meet a person in the community, and then some brief in-patient kind of stabilization, 24 hours, perhaps up to 72 hours. Again, we need to stretch these dollars to last the entire year and the crisis services are meant to assist anybody who is experiencing a behavioral health crisis, it doesn't matter if you're Medicaid eligible or not.
Ted Simons:
And another factor is housing and the transition to state-funded housing and those sorts of things. When does that start? Does that start immediately? What goes on here?
Laura Nelson:
We have a line item in the budget for supportive housing. Housing is not a Medicaid-covered benefit so we've always had to use state dollars to support adults with serious mental illness to keep them in a stable home. It would include services such as rental subsidies, maybe some utilities and that kind of thing, so right now there are several hundred individuals that are seriously mentally ill that don't qualify for Medicaid that are currently getting some supported housing services. Moving forward, the only people that we will be placing into supported housing settings will be Medicaid-eligible adults with serious mental illness. For adults currently on Medicaid in a setting like that we will continue to serve them and look at other alternatives and try to transition them out to another safe place to live.
Ted Simons:
When you talk about a safe place to live, you're not talking about temporary housing, hotels, these sorts of thing, homeless shelters. You're talking about safer environments, correct?
Laura Nelson:
Exactly. Do we not see a hotel or homeless shelter or support group home to be a suitable place in the long-term or permanent for an individual, so that would not be what we would consider an alternative placement.
Ted Simons:
But if things continue as they are, and if the money is stretched as it is, will they wind up -- some folks will inevitably wind up there, won't they?
Laura Nelson:
It is possible. If they lose that supportive housing, they will not be eligible to come back to that program, so we would have to look at other alternatives, what could they afford to pay out of pocket, do they have a friend, a neighbor, a sibling, a family member who could perhaps offer some support for them, as well.
Ted Simons:
The idea that some of the worse-care scenarios, hospitals, jails, simply on the street, realistic?
Laura Nelson:
I think it is absolutely realistic. There are many individuals I am convinced that are non-title 19 and have an SMI, serious mental illness that will do just fine as long as they can continue to have access to their medications. There, likewise, is another group we would consider very high risk, and we're going to be monitoring them very, very closely. We will be working individually with all of them to try to transition them as safely as we can. But we will be following to see what outcomes they have.
Ted Simons:
Last question. From where you sit with all of this going on and trying to handle and manage all of this and make this kind of adjustment and transition, what's the biggest challenge?
Laura Nelson:
I think the biggest challenge is trying to communicate the same information to as many people as we can. There are rumors just flying out there about who is going to get what, or when they're going to perhaps, you know have to transition out of their housing, and it's, I think, dealing with the, this very sad reality but not being paralyzed by it. We absolutely have to accept what we're dealing with and make the best decisions we can.
Ted Simons:
All right, Laura, thank you for joining us, we appreciate it.
Laura Nelson:
Thank you.
Dr. Laura Nelson:Acting Director, Division of Behavioral Health, State Department of Health Services;