New AI and insurance claims
April 1, 2025
A bill is making its way through the Arizona Legislature to stop the negative effects of AI on patients’ health insurance claims. House Bill 2175 would put safeguards in place to ensure claims are not arbitrarily denied by AI (artificial intelligence).
The Arizona Medical Association (ArMA) is backing the bill. AI is used in the medical world for health care, it is also used by insurance companies to review and deny medical claims.
According to the bill’s sponsor, Representative Julie Willoughby (R), who is also a registered nurse, HB2175 is among the first legislation in the nation to prohibit the use of AI in reviewing and denying claims for medical necessity and prior authorization requests.
The bill would guarantee cases involving medical judgment are reviewed by licensed medical professionals, individuals who have the training, experience and ethical responsibility to make clinical decisions.
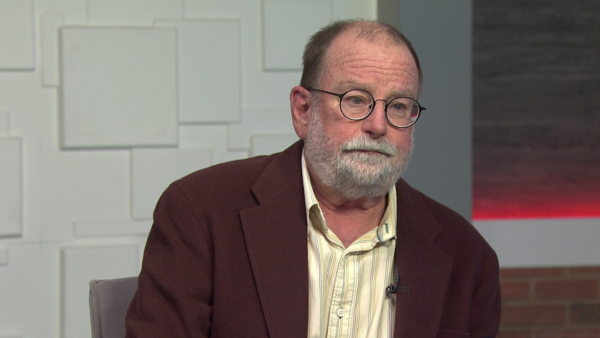
Dr. Michael Dunn, a Family Physician and ArMA Board Member, joined “Arizona Horizon” to talk about these claims and updates. Dr. Dunn is a family practice doctor in the East Valley.
“We’re seeing insurance companies are using artificial intelligence to review and some cases deny health care claims and prior authorizations. They mostly deny they’re doing this, but the evidence is starting to be somewhat overwhelming that they are,” Dr. Dunn said.
Can you spot AI’s footprint?
“Absolutely, “Dr. Dunn said. “Usually because the reasons for the denial are silly, and they don’t make a whole lot of sense. They don’t follow good medical judgment.”
“We had one last week. A patient came in, an occupational injury; she was bit by a cat, and needed to have the wound cleaned out. She needed a tetanus shot. And the insurance company, without getting into too much detail with the coding and stuff, we built an appropriate level of code to get paid for the visit. The insurance company sent back a denial or what we call a down code. And they downloaded it two levels, which represented probably $100 less in payment for us. When we read through what the explanation was, it was very clear a human had not reviewed that,” Dr. Dunn said.