Groundbreaking treatment targets glioblastoma with tumor-based cells
Nov. 4, 2025
Glioblastoma remains one of the most aggressive and lethal brain cancers, with few effective treatment options and an average survival of just over a year after diagnosis. Now, researchers at Banner MD Anderson have advanced to Phase II of a groundbreaking clinical trial using personalized immunotherapy made from patients’ own tumor cells.
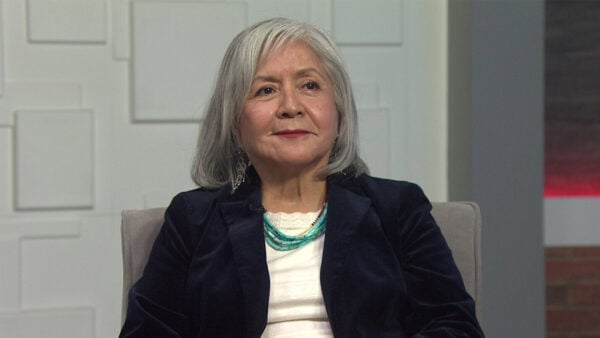
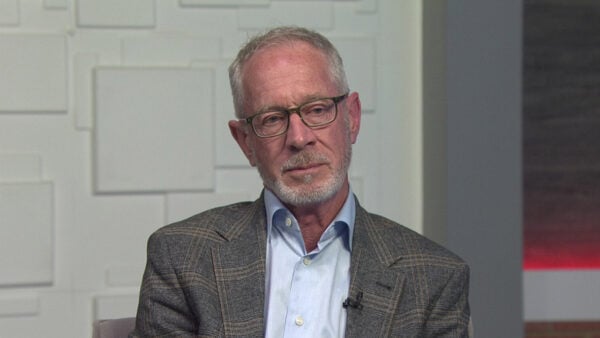
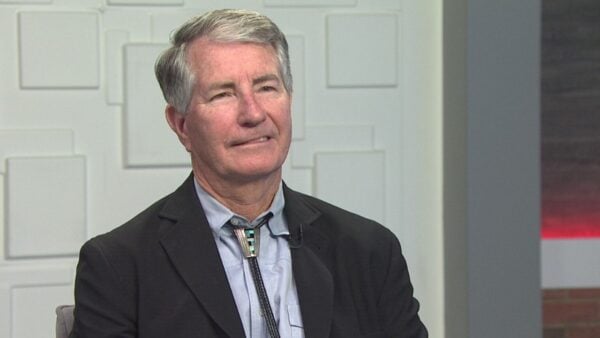
The approach is aimed at training the immune system to recognize and fight each unique cancer. Dr. Ramya Tadipatri and Dr. Joseph Georges joined “Arizona Horizon” to share how this experimental therapy works and what early results mean for patients and families.
Treating glioblastoma is uniquely difficult because the tumor adapts quickly and burrows into healthy brain tissue.
“The tumor can be pretty smart,” Tadipatri explained. “It mutates around the treatments we give, and glioblastoma especially can become resistant to many therapies.”
She added that the brain’s protective blood–brain barrier makes it even harder for the immune system to reach the cancer.
“This barrier can limit your body’s ability to send immune cells in,” she said.
Early detection can help, but only to a point.
“We ideally want to catch the tumor before it grows to the point of causing neurological symptoms,” Tadipatri said. “Once a patient develops these symptoms, it can be difficult to reverse.”
The Phase II trial builds on more than a decade of early research.
“Phase one is primarily designed to look at safety,” Dr. Georges explained. “Phase two starts looking more at efficacy—if the promising results we saw are really the case and if it’s really working.”
The treatment uses a patient’s own tumor to create a vaccine-like immunotherapy that trains the body to attack cancer cells.
“Our immune system has cells that can detect and attack cancer cells,” Georges said. “Glioblastoma is very good at tricking the immune system and hiding from it.”
But when researchers used tumor-derived antigens to create personalized vaccines, he said the results were unexpectedly strong.
“I started seeing MRIs where the tumor looked like it was melting away,” he noted. “For some of these patients… there wasn’t even a sign of tumor anymore for years.”
Unlike CAR-T therapies, which target a single molecule on cancer cells, this approach teaches the immune system to recognize the full range of tumor antigens.
“We don’t have to find that one target,” Tadipatri said. “The immune system is trained to respond to the whole tumor.”
The Phase II study will take two to three years to complete and has enrolled 23 patients so far nationwide. While early results are encouraging, Tadipatri emphasized the importance of rigorous testing.
“Average survival even with standard treatment is typically 12 to 14 months,” she said. Personalized approaches can extend survival somewhat, “but Dr. Georges can speak to seeing much better survival so far.”
Both doctors say they are cautiously optimistic.
“It appears to be very exciting right now,” Georges said. “We’re looking forward to seeing what the results will be.”