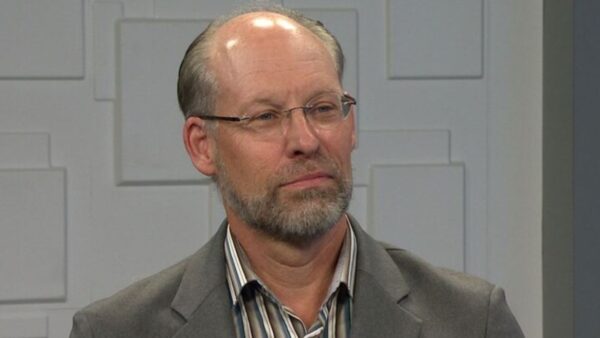
Responding to a court order in the decades-old Arnold v. Sarn lawsuit, Governor Jan Brewer has filed a proposal in Maricopa County Superior Court to make structural changes to Arizona’s behavioral health care system. Hear what Dr. Laura Nelson, Acting Deputy Director for the Arizona Department of Health Services Division of Behavioral Health and Anne Ronan, an attorney representing Arnold v. Sarn plaintiffs have to say about the Governor’s plan.
Ted Simons: This week governor Jan Brewer respond to a court order by filing a plan to improve Arizona's system of health care for people with mental illnesses. It's part of the lawsuit known as Arnold V Sarn, filed nearly three decades ago. As David Majure reports, lawmakers took time earlier this year to review the case that continues to shape Arizona's mental health care system.
Jan Brewer: This is a history lesson. I would suspect that they are not eight people in this legislature that really understand the history of Arnold versus Sarn it.
David Majure: It's a lawsuit that was filed in 1981 and the nation and the state were moving people out of mental hospitals into community-based behavioral health treatment.
Chick Arnold: I'm the institutional memory revolving around this case. I was a guardian as the Maricopa County Public Judiciary of 600 people with serious mental illness.
David Majure: He tried to help them obtain the community-based mental health services that were mandated by state law.
Chick Arnold: There weren't those Services in place. And with that, I became one of the five named plaintiffs in the center for law and the public interest effort to fix that.
David Majure: The case went all the way to the Arizona Supreme Court, which in 1989 affirmed that the state and Maricopa County have a statutory obligation to provide a wide range of Services for the seriously mentally ill.
Laura Nelson: Over the course of the lawsuit, as far as Services, it's been close to 2.2 billion dollars.
David Majure: Two decade and billions of dollars later, the lawsuit remains unresolved. Performance criteria required to end the lawsuit have not been met. And the company that manages Maricopa County's mental health system keeps changing.
Richard Clark: I am Dr. Richard Clark, the CEO for Magellan of Arizona.
David Majure: Magellan is the latest company selected as the regional behavioral health authority for Maricopa County. It was awarded a three-year, $1.5 billion contract in September of 2007.
Richard Clark: We do believe that significant gains have been made.
David Majure: But according to an audit conducted in 2008 by the court monitor assigned to the case, Services are declining.
Ted Simons: Governor Brewer hopes to improve the system by integrating physical and mental health care. She wants Access, Arizona's Medicaid program, to manager those programs for Access eligible adults. Other health clients and people with serious mental illnesses will still be served. The governor is also calling for a pilot program to serve the physical and mental health needs of people with serious mental illnesses through an integrated Service model. Joining me to talk about the governor's plan is Dr. Laura Nelson, acting deputy director of the division of behavioral health for the state department of health Services, and Anne Ronan, an attorney with the center for law in the public interest, which representatives the plaintiffs in Arnold v. Sarn. Good to have you both on the program. Let's get the basics. What is wrong with the way the state is care for mentally ill patients?
Laura Nelson: I think it's important to start out by -- to back around to the Arnold lawsuit and remember that that lawsuit is focusing only on the adult population with serious mental illness. That is the population that seems to be most in focus and under discussion around the state. The children's system has been let scrutinized of late, and the Services for general mental health adults and adults with substance abuse. The concerns that have been raised around working with the adult population that has serious mental illness lives back to the expectations and the court orders related to the lawsuit. And the various administrations that have been in place, the various providers that have been in place and the various regional health authorities that have been in place have at come out with -- at this with the same goal. We all have the same goals in mind, including that of the plaintiff and the monitor. We really want people to get the best care possible. It's how we go about structuring that system to make that happen and how we monitor appropriately to see that the outcomes are being achieved, has been at the crux.
Ted Simons: Why are the outcomes not being achieved? What is wrong with Arizona's mental health care system?
Anne Ronan: Well, from our perspective and when the most recent audit came out towards the end of last year, early 2009, we stepped back and said why do we continue to see the outcomes not be good, not be what people are expecting? Primarily the biggest concern was that the monitor's audit continually showed that the persons with serious mental illness needs were not being met. Which is the fundamental purpose for the behavioral health system, to meet the needs of these folks. What we feel quite strongly is that there are too many layers of infrastructure in the system in Maricopa County, and it makes it very difficult to actually hold anyone accountable for quality of the Services delivered. There are providers that have direct contact, there are Reba directors, then the state office at the department of health, and then there's the Access administration for that part of the population that are Medicaid eligible and very, at every given point somebody can say it's not really our fault things didn't work it's the folks below us or above it. We were advocating for fewer layers, direct responsibility from the state office to the consumer.
Ted Simons: It sounds as if the governor's plan has consolidation here. Access takes care of mental and physical care. Does that not get rid of some of the layers you're concerned about?
Anne Ronan: The proposal has the population of persons with what they call general mental health and substance abuse issues being transferred to "The Arizona Republic" health plans. It doesn't deal with the population that is the subof the Arnold lawsuit except are in a pilot. We don't actually -- we don't actually see from the pilot and from what little we know about the pilot, that there is actually going to be a change.
Ted Simons: Is that a legitimate argument, that the governor's plan focuses on an area that needs less focus than another area?
Laura Nelson: I think the governor has done a lot of work in the last eight months. She's met with various stakeholders, including plaintiffs and the monitor in the case, she's left with other regional behavioral health authority representatives, providers, advocates, she and a small group of legislators did their due diligence to gather as much education -- as much information as they can to educate themselves about what's working and what's not working in the system. They use that information to look at numerous options, and this was the decision that the governor made as being the best approach at this time.
Ted Simons: There are some critics, though, that say when you consolidate this mental and physical health care system in the way the governor has proposed, when other states have done this the results haven't been so hot . Is that a valid argument?
Laura Nelson: I think certainly part of the reason for wanting to do this as a pilot rather than wholesale move, physical health and behavioral health together is so we can absolutely take am good assessment and evaluation of what those outcomes would be. If we can structure our system in a way that we do achieve better physical health care as well as behavioral health care outcomes, we would be able to move forward. But I think she's being smart and wanting to pilot this project here in Arizona to see if we can achieve good outcomes.
Ted Simons: Does that make sense? Go ahead with a pilot program, see how it works, take it from there.
Anne Ronan: The problem with the pilot program is that first we don't know how many people are going to be included, but if we can assume it's not going to be most of the people, it's going to be a smaller number of the enrolled persons with serious mental illness, the pilot itself wouldn't even be operational in the best case scenario until sometime a year from now. The plan is to study the pilot for a couple of years, once it gets rolling, and in the meantime for thousands of persons with serious mental illness, there will be no change. And that is a very serious concern to us. Because we believe there needs to be a restructuring and greater accountability for the whole population. And to wait three years is not acceptable.
Ted Simons: Can you respond to that? Does that sound like -- did that make sense to you?
Laura Nelson: Ted, I'd like to respond to that. I think one of the things we need to keep in mind is that when the current provider, Magellan, came on board, they responded to a drastically different request for proposal than had been in place of that. Proposal was developed after consulting with the community W. stakeholders, with plaintiffs to talk about how we could restructure the system at that point. So we are already in the middle of and finishing a pretty significant restructuring process. The regional behavioral health authority has spent the last two years contracting with community-based providers to actually run the SMI Clinics here in Maricopa County. Previously the contractor themselves was directly responsible for those Services. So there has already been a significant restructuring that's taken place. It's important to also not assume that time has stood still since the last review of the system was done. There has been an enormous amount of effort going into establishing dashboards, looking at outcomes, increasing the staffing ratio, looking at the quality of the Services in the system.
Ted Simons: One of the problems I think we all have with covering this story, we're not quite sure what the pilot program entails. There's a lot of mystery there. Can you help us with that?
Laura Nelson: We can certainly talk a little bit about some of the issues that convenient identified. We had a good meeting yesterday where we started to talk about some of those topics that have come up. And they still need to be hammered out. Part of the process is going to be establishing a task force with the expertise at the table that can help walk through the things you need to think about. But as Anne just mentioned, there's questions as basic as how big will the sample size be? How many people will be enrolled? How will you ensure have you a representative group of individuals that are participating? What sorts of outcomes will you be looking at? How will you evaluate that? How will you fund this pilot?
Ted Simons: Do you have enough -- are you getting or do you think you will get enough information on this pilot program to get a better sense of what's going on here?
Anne Ronan: Well, I think definitely over the next couple weeks we'll get more information about the pilot program. But our concern is that by its own design, it's not going to result in change for over three years. I mean, that's how it was explained to us, that's the design.
Ted Simons: We've got a couple minutes. Give me a scenario, a patient, the patient in the system right now, a patient in the system as the governor wants to see it. What's the difference? What changes?
Anne Ronan: Well, we're not really sure except that there would be an entity who would be responsible for their mental health Services and their physical health Services, it would be -- in theory it would be the same organization. You mentioned earlier in some states this is not worked. And they've had some bad experiences in other places. One of the things that has happened when you're talking about such a big system is that could you just as easily get a large managed care plan that does the medical -- the physical health, subcontracting with Magellan or value options which would give us the same system we currently have in Maricopa County. Not real integration, just bigger providers contracting together.
Ted Simons: Is that not a concern to where folks would have much more experience on the physical health care side, and the mental health care side kind of gets the shortened of the stick?
Laura Nelson: Absolutely that's a concern. I know the governor has that concern as well. She's been extremely supportive of behavioral health, and I'm sure that one of the aspects of this whole pilot would be that behavioral health care not be overlooked. And it's important to acknowledge the research that's been done lately around morbidity and mortality for adults with serious mental illness. Individuals across the country are dying 25 -- in Arizona 30 years younger than the general population because they're not getting basic physical health care that everyone else is having access to.
Ted Simons: All right. We have to stop it right there. Great discussion. Thank you both for joining us tonight on "Horizon."
Anne Ronan / Laura Nelson: Thank you.
Dr. Laura Nelson:Acting Deputy Director, Arizona Department of Health Services Division of Behavioral Health; Anne Ronan:Attorney representing Arnold v. Sarn plaintiffs;