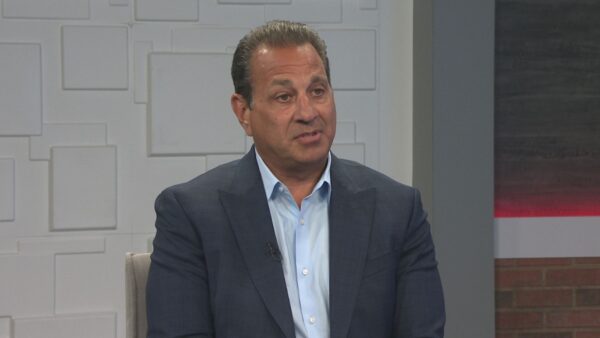
In light of the recent shootings in Tucson, the state’s division of behavioral health has developed a mental health checklist that provides assistance and information to those that believe someone they know needs help. Dr. Laura Nelson, director of the Division of Behavioral Health, Arizona Department of Health Services, discusses.
Ted Simons: In light of the recent shootings in Tuscon, the state's division of behavioral health has developed a mental health checklist that provides assistance and information to those who believe someone they know needs help. Here to tell us more about the checklist is Dr. Laura Nelson, director of the division of behavioral health for the Arizona department of health services. Good to see you again. Thanks for joining us. Let's talk about this thing. What is this specifically designed to do, this checklist?
Dr. Laura Nelson: The idea is to make it as easy as possible for anyone who visits our website to understand how to navigate through the system, depending on the severity of the symptoms that they're seeing.
Ted Simons: So how -- How is it developed? How do you know which direction to take people, this way, that way? It's kind of a flow chart isn't it.
Dr. Laura Nelson: It is. It's more of a flow chart than a checklist. But the idea, I think where most people intuitively understand the most is at the top, if you feel that you are immediately in danger of being harmed or that someone else is at risk for being harmed, call 9-1-1. You always should do that. If you come upon a bad automobile accident, you call 9-1-1. Or if someone is trying to break into your house, call 9-1-1. So in any situation in which you feel unsafe, that's always an option. Where I think folks have perhaps not necessarily had the information at their fingertips that we feel would be most hopeful is really when you're not going to call 9-1-1 and get the police involved. But there are crisis numbers available in any region of the state, and we have those easily accessible here on this website. If I'm in Umatilla County, what crisis number do I call? Through calling a crisis line, you're accessing behavioral health professionals who may be able to successfully intervene right over the phone, they may decide that they need to send out a mobile crisis team to come to you and talk with you further, or they may say, in this situation, I don't think you really need us, but let me help you figure out what might be more appropriate, because it may not be at that level where you actually need a crisis intervention. And that's where we get to, I think, the most exciting part of this flow chart. Really helping family members, neighbors, colleagues from work, classmates, or teachers really understand what they can do to intervene earlier rather than later.
Ted Simons: We're looking at flow chart right now. It really is very easy to figure out, and basically if you can answer one question, you either go down a level or to the side on a level, and these sorts of things. It's really something. It's very well done. But you kind of wonder, once you're there, you can figure it out pretty well, because it's very well done. How do you know to get there?
Dr. Laura Nelson: That's where you come in. We want you to get word out in terms of our website, and we've been trying to advertise this through all of the networks that we have. Now, we are most typically involved with the public behavioral health system, and we have networks where we can get this information out. But we want this website to also reach out to anybody that is in Arizona, regardless of if they're part of the Medicaid system, there are people that have private commercial insurance or veterans that could benefit from knowing about this information. So we're really trying to reach out to the media and to the public to let them know that this resource is available, and if they have thoughts on how we can improve it to please let us know there. There are probably gaps in here that we would like to be able to fill in.
Ted Simons: Talk to us about real quickly the facts and the myths of mental illness. I know that's part of the website as well. Things more common than perhaps people might imagine, mental illness is, and what involuntary treatment means.
Dr. Laura Nelson: Exactly. Well, you hit on a very good point. One in four adults in a given year is experiencing a mental illness. So it is very alive and well in our country. And internationally. In fact, most people that do struggle with a mental illness are experiencing symptoms gradually over time, and you would be surprised how if you're looking for it, as somebody who knows that person well, your best equipped to recognize when something seems to be changing and how do you then engage that person in conversation? But some of the myths really have -- and we've seen them a lot since this tragedy in Tuscon, we continue to hear this myth about how people with mental illness are violent. And that's absolutely not true. And one of the biggest concerns Ted that I've had as a result of what has happened has been what is the impact that this kind of attention is having on people who are receiving treatment in our system, and are hearing kind of this reaction and it's just further stigmatizing and discriminating against them, and they're the ones that have actually sought treatment and are on their way to recovery.
Ted Simons: It's almost a double-edged sword raising awareness, it's good that people are out there learning more and finding out more, but it's also a little bit of a concern because now all sorts of ideas are floating and you got to get to a website like this to get the real deal.
Dr. Laura Nelson: And part of the myths that need to be debunked are that people with mental illness actually can recover with the right support and treatment, they really can do very, very well. They can get jobs, they can contribute to their community. And so one of the other double-edged swords as you talk about and mentioned a minute ago, has to do with the involuntary commitment process. And the idea here is how do you encourage someone to seek treatment voluntarily and realize that they could benefit from treatment? If you -- and there are times when you may need to, but the more you push for the involuntary forceful entry into treatment, the more you just reinforce why somebody doesn't want to be there.
Ted Simons: Last question before we let you go, obviously the Tuscon shootings, major, major story. What kind of calls are you getting, the volume of calls? Has it just been as much as we anticipated?
Dr. Laura Nelson: Yes. I think it has been. We've set up a support line both in Tuscon, to specifically help that community, and then we set up another 1-800 number for the rest of the state. The two lines the last count I received was about 550 to 560 calls from people around the state who either wanted to talk about trying to process this, offer help, one of the other kind of scary things that we heard from some individuals is that the trauma in Tuscon was bringing up painful traumatic experiences and memories for them, from previous traumatic events.
Ted Simons: Well, all right. Good work, we'll talk more about this in a little bit down the road. But at least it's up there and people know what it's about, and it's good to have you on to talk about it.
Dr. Laura Nelson: Thanks for helping us get the message out.
Dr. Laura Nelson:director, Division of Behavioral Health, Arizona Department of Health Services;